Dr Andrew Mackay, ACP GP Advisor to the Edinburgh Health and Social Care Partnership ACP team.
“Definitely thinking back to those days where people were not thinking about these kinds of things. We were not always doing the right things for the residents, the appropriate things.” Care home staff member.
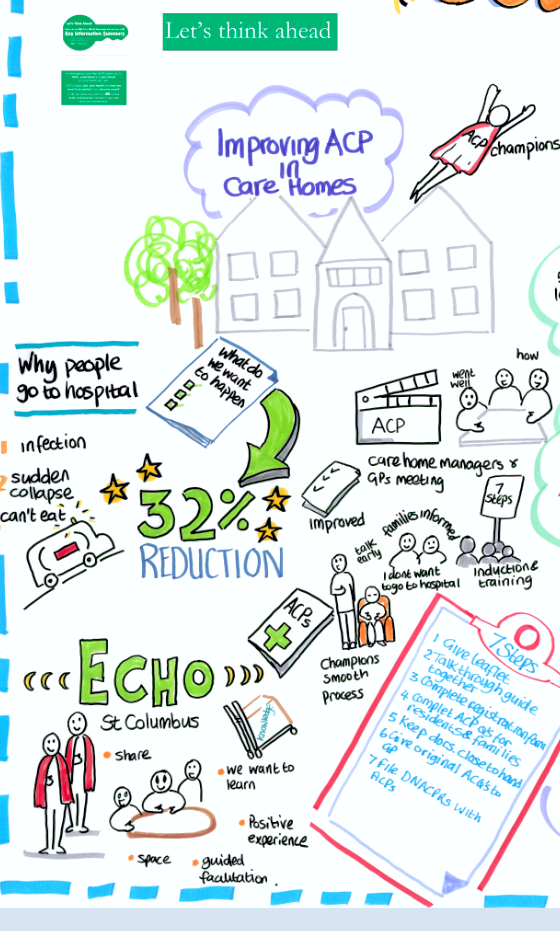
For the last year I have been working as part of a team to embed Anticipatory Care Planning (ACP) in 20 care homes across Edinburgh. Like the staff member above, many people involved in looking after care home residents appreciate that admission to hospital is not always what the resident wants when they are acutely ill. Some just really don`t want to go to hospital at all and others feel that their quality of life is now such that if they were seriously ill they would prefer to be kept in the home they know with treatment being provided there, even if that meant they couldn`t get all the possible treatments for their condition. We were keen to see whether training the care home staff in how to discuss ACP`s with their residents and how to use the completed ACPs in an emergency would reduce the number of avoidable admissions to hospital.
The care home staff immediately got it. They all want to provide high quality person centered care and they hate to see residents ending up in hospital when it is unlikely to help them. When this did happen many staff felt as if they had somehow failed their residents. What is more, many of them were already having conversations about the future, but they found them difficult at times and didn’t know how to use this information in the best way. The GPs were also delighted to get some help with gathering the information they needed to create a high quality ACP. They all wanted to do their best but had been overwhelmed with the time needed to do it properly. The idea that the person having a ‘good conversation’ with residents or relatives with someone that knew them well seemed obvious to everyone. In most situations that person was a member of the care staff.
The staff were really positive about the tools we showed them that together comprise the ‘7 Steps to ACP for Care Homes’. They were brief, simple and included lots of explanation. Although anxieties still remained. Much of the time people arrive in care homes from hospital, where they have been pretty unwell. They and their relatives are going through a huge readjustment. Trying to figure out the present is a challenge and thinking about how to direct future care seems impossible to some when they are new to the home. For some, even when the initial dust has settled conversations about their or their relative`s plans for the future are still not easy. I have been having these conversations with care home residents and their relatives for years and sometimes I still don`t get it right. Our trainer was able to work with staff to help with this. It can be really useful to have a few phrases you are comfortable with to help introduce the subject and to be able to back that up with some written explanation.
Getting the GPs on board was also pretty straightforward. They saw immediately the logic of the system we offered and we were also able to help train some of their admin staff to take on the basic data entry. As one practice manager said to us: “If it is an admin task that needs to be done, please don’t ask the GPs to do it. Our team does it much better!”.
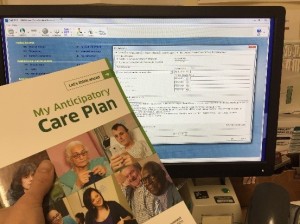
So, the questionnaires were completed and passed to the GP, the ACPs were entered as special notes in the residents Key Information Summary (KIS), that form was printed and returned to the care home. The next big challenge was using the ACPs in an emergency. Whenever a resident becomes suddenly acutely unwell it is scary for those looking after them. Particularly when we started, some staff would feel better calling for an ambulance. Through work with our trainer they became confident in using the ACP to guide their actions and to help guide the actions of out-of-hours doctors and ambulance crews. It was really useful for the staff that we helped them complete reflective logs of each of the acute events and then met with them to discuss all the episodes every 6-7 weeks. It was a happy coincidence that many nurses needed to complete reflective logs for revalidation so were keen to do it with our help.
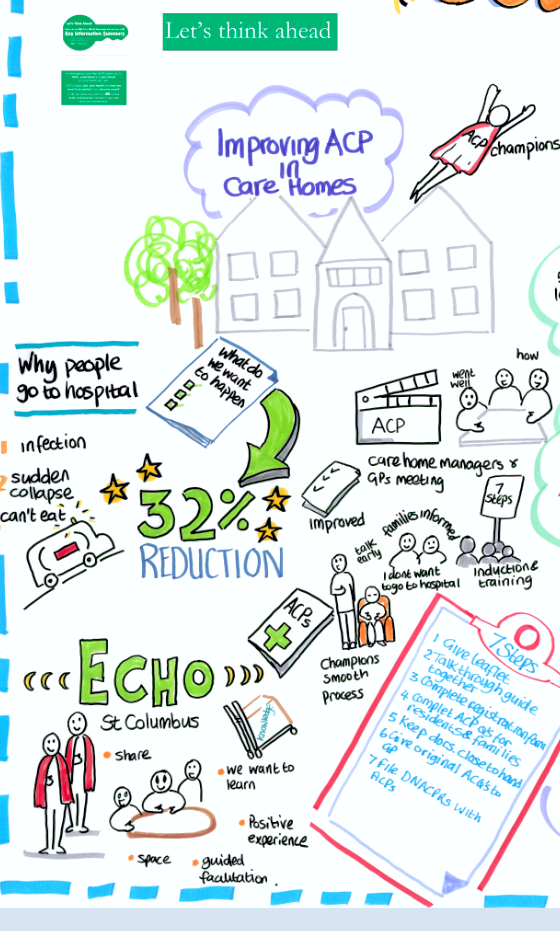
Care home staff are busy people and I often worried that they would struggle with what was, in some ways, extra work. So it was wonderful at our recent end of program celebration to see so much enthusiasm from the staff about ACP. Person after person thought that this process had helped them deliver far better care for their residents. It was heartening to be able to share with them that there had been a 32% reduction in potentially avoidable admissions to hospital from their homes over the first ten months of the programme. However, I was even more pleased to see just how positive they were. It gave me a lot of hope for the future. Talking of the future, I now really hope we can sustain them. Some care homes have up to 30% turnover of staff so the effect of other programs has faded over a few years. We have tried to address this by recruiting several `ACP Champions` in each home and training them to carry the message onwards. We’re also developing an implementation package to support the ‘7 steps’ toolkit with training material, videos, leaflets etc.
“…ACP is a very good programme for us to do our job as expected from us” (Care home deputy manager).
“The ACP pathway helped. It helped tremendously. I don’t think we would get anywhere without using it. Explaining each stage more fully to the resident, and he understood why we were asking. He said it was a relief and a comfort to talk about it.” (Care home champion)
“I find that staff are initially shocked that someone might not want to go into hospital for treatment and might want to be kept comfortable in the care home. It’s been really important in providing us with confidence to speak about what people’s wishes are if they become really unwell.” (Care home champion)
“If you want to enhance your practice you have to buy-in to this process. We are supporting person-centred care and this supports us from the very beginning. They’re telling us what they want and we are here to facilitate that.” (Care home manager).
Long may it continue and let`s spread the word.
Written on behalf of the Edinburgh Health and Social Care Partnership’s Long Term Conditions Programme ACP team.
For more information and resources relating to ACP visit the ACP toolkit.
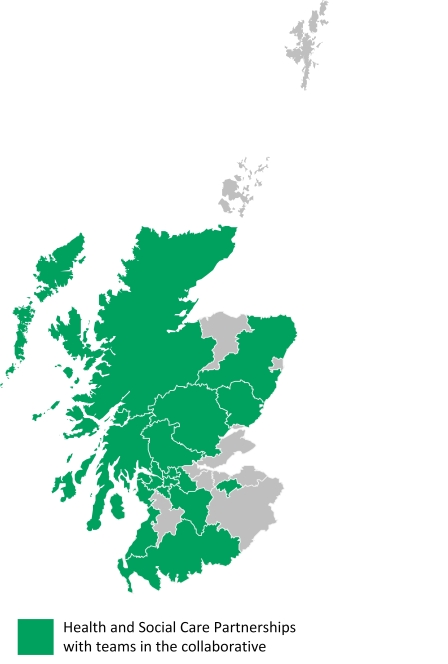 HSCPs with teams in the collaborative:
HSCPs with teams in the collaborative:

 Anticipatory Care Planning is not a one-off event. It is a process that starts with a conversation and which can develop and evolve over time. The beauty of general practice is that we have opportunities to initiate that conversation and contribute to the development of an ACP over weeks, months and sometimes years.
Anticipatory Care Planning is not a one-off event. It is a process that starts with a conversation and which can develop and evolve over time. The beauty of general practice is that we have opportunities to initiate that conversation and contribute to the development of an ACP over weeks, months and sometimes years.