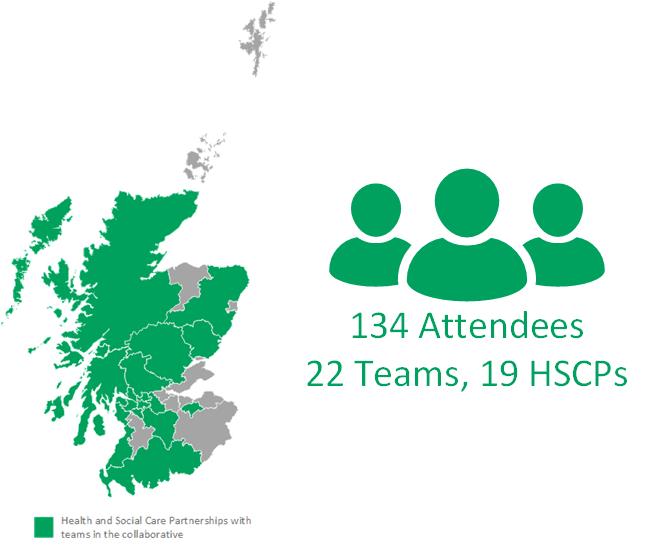
On 27 February 2020 we were joined by Away Team members from the 22 teams taking part in the Living and Dying Well with Frailty Collaborative. Teams travelled from across Scotland to come together for the second learning session where they learnt about the theory of complexity and the recently published Framework for Community Health and Social Care Integrated Services and considered how this impacts on their work. Teams also spent time sharing and learning from each other’s progress and experiences of implementing their ideas since the first learning session. They then had time as a team to discuss what they had learnt and develop their plans for the next action period.
We had a great turn out on the day and mixture of representatives from the Away Teams:
Setting the scene
The theme for the day was bridging the gap between practice and strategy. We spent the morning focussing on understanding the system, with the afternoon shifting to what teams are doing within that system.
This was brilliantly introduced with an example from Iain Ramsay, National Professional Lead for Social Services with Healthcare Improvement Scotland, who discussed his experiences of the Virtual Community Ward in Aberdeenshire. Absolutely key to any work like this is the building of relationships. This is at the heart of what we are trying to achieve to improve outcomes for people with frailty through this collaborative approach. Working in a health and social care system is complex and can be perplexing and very challenging. Improving services cannot be done on a one size fits all basis, but there are real advantages to testing and implementing in collaboration with other teams and learning how they have approached and overcome similar challenges.

“Our Social Work advisor (Iain Ramsay) sets the tone. Success: ”It’s pretty much all about relationships”. How true. Looking forward to building on some today” (tweet from attendee)
Understanding the system
The morning session was packed full of thought provoking information and theory. This included a comprehensive walk through of the newly published Framework for Community Health and Social Care Integrated Services and how this could support the design, development and delivery of services for those who are living with frailty. This was an excellent and engaging presentation littered with real life examples by David Rowland, Professional Adviser at Scottish Government. If you would like to know more about the framework, you can watch a recording of the presentation here.
Following this Ruth Glassborow, Director of Improvement at Healthcare Improvement Scotland, gave an engaging talk on complexity theory and how we may need to use different strategies with different problems. The further ahead we look the harder it is to predict what could happen. One tool that may help you to assess your situation more accurately and respond appropriately is the Cynefin framework. This is a problem-solving tool that helps you put situations into five “domains” defined by cause-and-effect relationships.
“What is my style? How do I interact with those who have a different approach or style? It is really obvious to me that there are PROCESS people and RELATIONSHIPS people. I know very few who have mastered both” (comment from attendee)
The morning was wrapped up by Dr Paul Baughan (National Clinical Lead for Palliative and End of Life Care) and Professor Graham Ellis (National Clinical Lead for Older People and Frailty) who looked at complexity and anticipatory care plans (ACPs). By this point there was definitely a theme emerging about cats!
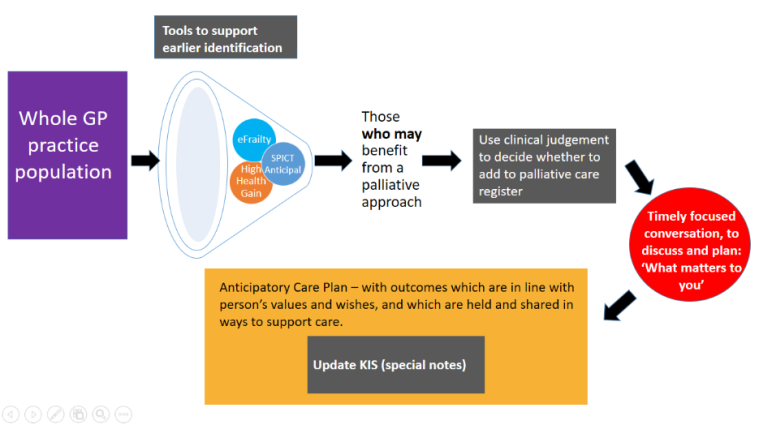
There is a growing evidence base that ACPs and key information summaries (KIS) lead to positive outcomes, with a recent article in the British Journal of General Practice highlighting that the chances of dying in a community setting were 3.7 times higher with a KIS than without one (Finucane et al, Dec 2019). However, there is huge variation in the percentage of the population across Scotland who have a KIS, and this is partly due to the complexity of the process. Here are just some of the reasons people give for not completing an ACP:
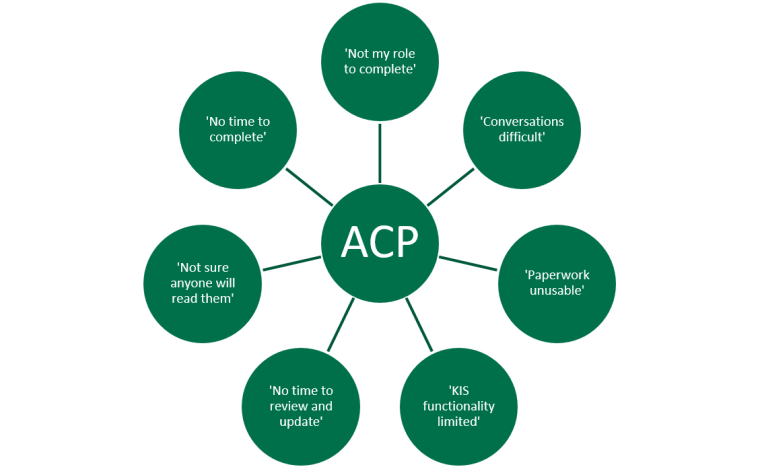
Teams had the opportunity to discuss this issue and think how they can apply this to their work during the next stages of the Living and Dying Well with Frailty Collaborative.
What the teams are doing
We wanted the afternoon to be focused on time for teams to come together and learn from each other’s successes and challenges and get the support they needed to move forwards. The teams were split across four rooms and each took turns to share their experiences with each other using presentations they had prepared in advance, with some time for questions and discussions. There was some great learning between teams on the different approaches being taken, and reassurance that people are facing similar issues and challenges. The networking opportunities offered will allow teams to continue to share their learning with each other over the next stages of the collaborative.
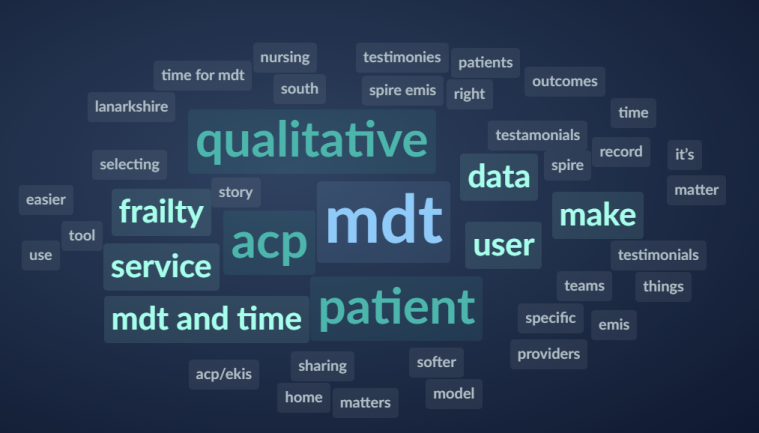
This was followed by more in depth discussions on topics that the attendees self-selected via unconferencing. We wanted to put improvement into action and practice what we preach, so ran a test of change to ask attendees to submit the topics they wanted to discuss in more detail into Sli.do. This produced a word cloud from which key themes could be identified and attendees could choose which of these topics to join a conversation on. An example of a word cloud generated on the day can be seen below, and key information from the topics discussed in each room can be found here.
We wish we had more time on the day to devote to sharing of learning and discussions, but hope the mixture of theory and discussion was valuable to all who came and will help inform the next steps of the teams.
Teams were then given time to work together to plan the next steps for their team to undertake during the second action period.
If you are undertaking similar improvement work you may find the below resources helpful:
- QI Zone including E-learning modules and tools from NHS Education for Scotland
- Action planning template
- Improvement pause template from Scottish Improvement Science Collaborating Centre
- Huddle guidelines
- PDSA template
What next?
During the second action period Away Teams will share their learning with the Home Teams and work together to collect and submit data and progress reports. They will be supported by the national team at Healthcare Improvement Scotland and encouraged to continue to share their learning with each other.
For more information about the collaborative please visit https://ihub.scot/improvement-programmes/living-well-in-communities/our-programmes/living-and-dying-well-with-frailty/

“Finally home after a brilliant day at LWiC Frailty Collaborative. A day spent learning, networking and planning for the future. Amazing what you can achieve when you work collaboratively across all sectors of care.” (tweet from attendee)
Covid-19 update – 16th March 2020
Since the learning session we have seen a rapid escalation of the Covid-19 outbreak across Scotland. Healthcare Improvement Scotland has taken the decision to place all national improvement support on hold until later in the year. We have made this decision for two reasons:
- We do not want to place any additional pressure on services at a time when they are heavily involved in preparing for and responding to COVID-19.
- We will be temporarily refocusing our improvement resource to support work aligned with COVID-19 resilience.
This means that Learning Session 3 on Thursday 4th June is now cancelled. If you have any questions please do not hesitate to contact the Living Well in Communities on: hcis.livingwell@nhs.net.
Please be aware that this is a rapidly changing situation. Please check our website for more information. You can also find more information on Covid-19 at NHS Inform.


 Here’s a short introduction from Paulo Nunes de Moura, who has recently joined the Living Well in Communities team.
Here’s a short introduction from Paulo Nunes de Moura, who has recently joined the Living Well in Communities team.


 Calvin’s recording studio for the day was Dollar Health Centre, where Paul works as a GP. His set up is fairly minimal: a USB microphone plugged into laptop to record the audio, and headphones to check the sound. The podcast format is an intro from Calvin, an interview with his guest speaker, and a recap of key learning from the podcast at the end. This really reinforces potential of the podcast for sharing knowledge and getting it into practice.
Calvin’s recording studio for the day was Dollar Health Centre, where Paul works as a GP. His set up is fairly minimal: a USB microphone plugged into laptop to record the audio, and headphones to check the sound. The podcast format is an intro from Calvin, an interview with his guest speaker, and a recap of key learning from the podcast at the end. This really reinforces potential of the podcast for sharing knowledge and getting it into practice.





 “Fantastic reasons to be at #LWiCFrailty today. But “a goal without a plan is just a wish” so now time for action! Thanks for a useful day of sharing & learning @LWiC_QI @eFI_Midlothian”
“Fantastic reasons to be at #LWiCFrailty today. But “a goal without a plan is just a wish” so now time for action! Thanks for a useful day of sharing & learning @LWiC_QI @eFI_Midlothian”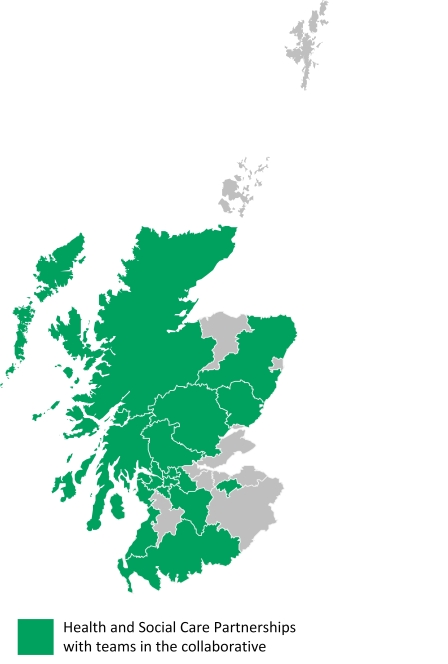 HSCPs with teams in the collaborative:
HSCPs with teams in the collaborative: My mum lives eight hours away, within earshot of Glastonbury (if only her hearing was a little better). Her frailty is a pressing reality. All of the issues which press in at work – frail older people, most with a host of health issues, increasingly lacking capacity, exhausted family carers, stretched paid carers, the role of GPs, district nurses; it all feels very personal.
My mum lives eight hours away, within earshot of Glastonbury (if only her hearing was a little better). Her frailty is a pressing reality. All of the issues which press in at work – frail older people, most with a host of health issues, increasingly lacking capacity, exhausted family carers, stretched paid carers, the role of GPs, district nurses; it all feels very personal.