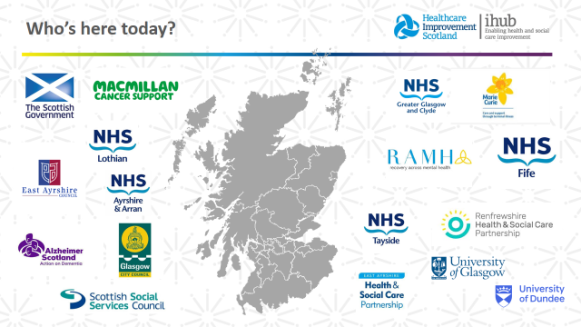
At the end of August 2019, we were joined by representatives from national and local organisations with a passion for good palliative and end of life care. They had come together to help us explore how we could make a positive difference to the palliative care received by people who lived in care homes.
We had a great turn out and mixture of representatives from organisations including (although not limited to):

We were brilliantly supported with facilitation on the day by colleagues from the Care Inspectorate.
Background
During phase one of Living Well in Communities palliative and end of life care work we supported local testing to improve the identification and care coordination of people with palliative and end of life care needs. There have been some great learning and outputs from this work, in particular around the care home setting. We are also aware of some of the wonderful resources and initiatives that exist, or are being developed and want to find out more about these and other areas of work.
We are currently in phase two of this work – scoping and understanding how we can take the learning from phase one, and from other areas of good practice, and spread them across Scotland. To achieve this we are exploring the potential of delivering an improvement collaborative. In an improvement collaborative we would work with staff, to understand the interventions/models of care that would help them to improve outcomes. Following this we would support them to: put these into practice, understand the difference they have made, embed and spread their learning.
At the moment we are seeking to understand the context, challenges and initiatives underway in care homes. A key part of this is to explore how an improvement collaborative could work in practice. We recognise that it is important to be clear on our offer so that we can engage meaningfully with staff delivering care, residents, families, and carers (informal and formal).
You can find out further information about the background to this work on our website and by reading the blog post about our meeting with Care Inspectorate colleagues.
What have we found so far?
 Paul Baughan, GP and national clinical lead for palliative and end of life care, provided a great introduction to the workshop with an interactive ‘blockbusters’ presentation using data about care homes ( taken from the Scottish Care Home Census available from Information Services Division (ISD) website) to help set the scene and provide context for the workshop.
Paul Baughan, GP and national clinical lead for palliative and end of life care, provided a great introduction to the workshop with an interactive ‘blockbusters’ presentation using data about care homes ( taken from the Scottish Care Home Census available from Information Services Division (ISD) website) to help set the scene and provide context for the workshop.
Following this we had good table top conversations on some of the themes that had emerged from engagements so far, getting feedback on what was important and was what was missing. We are using this feedback, as well as other, to inform our work in phase two and will be looking to share this in the future.
Building the picture
The main focus of the workshop was a world café session, where attendees were asked to help us understand what we need to consider as we develop our approach and plan for this work. The topics and key points emerging were:

Stakeholders
There was a good discussion highlighting the broad range of staff and organisations contributing to the care and support of residents, in particular identifying:
- It won’t be possible to engage with everyone so we need to be clear on focus of the work to help prioritise who we reach out to.
- There is a need to promote the stories of the good palliative and end of life care people are having in care homes to dispel the negative perceptions around these areas.
 Language
Language
The group looked at some of the language used in relation to end of life care, with some interesting reflections on the subjective meaning to some of the terms. Some of the general reflections were:
- Staff can be nervous about the associated language and what they are recording as “end of life” or “palliative”.
- It is important to ensure that language is tailored to the audience and framed around the key things that is important to them.
 Scope
Scope
Attendees provided valuable insights into what should be in and out of scope for the proposed work, including consideration on settings, change ideas and what areas that should be scoped further. Other areas included:
- The important role of the Health and Social Care standards in framing this work.
- The need for targeted exploration to understand the issues faced by different care home providers and also understand the challenges being faced by the workforce.
 What will help or hinder our success?
What will help or hinder our success?
There were interesting discussions highlighting that certain elements could be seen as either helping or hindering depending on how they were interpreted and implemented. Some of the key points were:
- The role of leadership in supporting this work and giving and sustaining permission (empowering) staff.
- The need to ensure a balance of adapting and adopting good practice that is responsive to local need but does not lose the essence of what it’s about.

Good practice
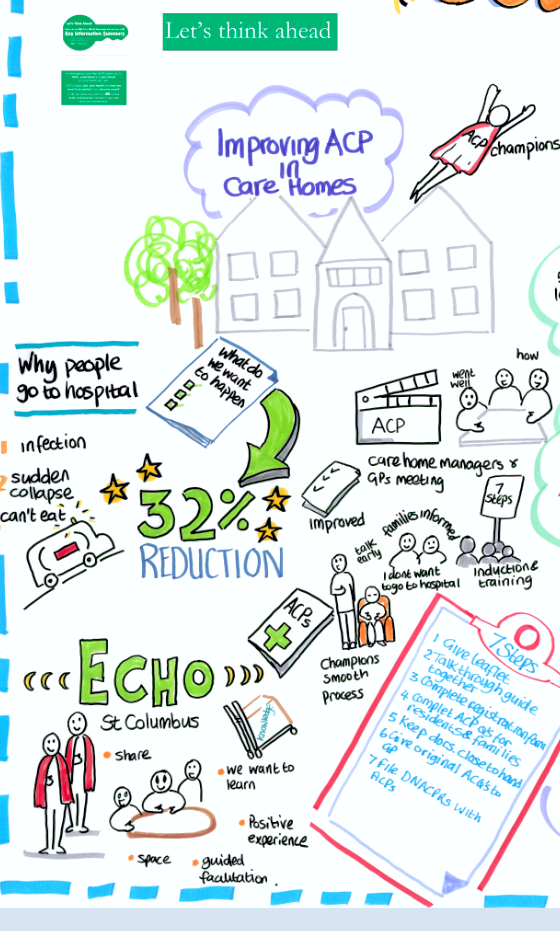
We were keen to find out about other initiatives that were making a positive difference, some of those that were highlighted were:
- Developing staff understanding and skills in relation to palliative and end of life care (MacMillan Foundation).
- Utilising technology for learning and peer support (Project Echo, Strathcarron Hospice).
- Use of dedicated care home link with Advanced Nurse Practitioners/ Nurse Practitioner/District Nurses (Aberdeen City, East Lothian, Fife, Glasgow City, Western isles HSCPs).
- Providing training and utilising tools to assess and respond to an individual’s palliative care needs (Glasgow City HSCP).
- Anticipatory Care Planning questions in care homes (City of Edinburgh HSCP).
What did people think about the workshop?
“Great chance to network and find out what is working well in care homes in other areas, good to hear different views and find out more about what other organisations do”
Feedback was positive, with attendees enjoying the opportunity to network with like-minded individuals with an interest in palliative and end of life care. The workshop was interactive and allowed attendees to hear about existing work underway in care homes. However, it was felt that there is a need to be clearer about the objectives and overall outcomes this work is looking to achieve, and to ensure that the experiences and voices of care home staff and residents were at the core of this work moving forward.
Next steps
It is important get this work right and we want to invest time we want to work with partners to understand how we can make a positive difference to the palliative and end of life care experienced by care home residents.
We are reviewing all of the outputs from the workshop and our engagements so far and will use these to help us refine our focus and approach. An important aspect will be using this intelligence to help us meaningfully engage with the key groups and people, including care home staff, residents, families, and carers (informal and formal).
Finally, we’d like to share a big thank you from the Living Well in Communities team to everyone who attended and contributed to the workshop.

Please visit our website for further information https://ihub.scot/living-and-dying-well-in-care-homes/





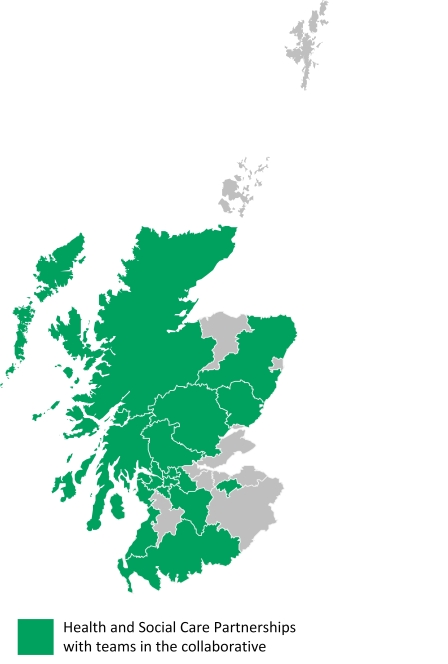 HSCPs with teams in the collaborative:
HSCPs with teams in the collaborative:




 My mum lives eight hours away, within earshot of Glastonbury (if only her hearing was a little better). Her frailty is a pressing reality. All of the issues which press in at work – frail older people, most with a host of health issues, increasingly lacking capacity, exhausted family carers, stretched paid carers, the role of GPs, district nurses; it all feels very personal.
My mum lives eight hours away, within earshot of Glastonbury (if only her hearing was a little better). Her frailty is a pressing reality. All of the issues which press in at work – frail older people, most with a host of health issues, increasingly lacking capacity, exhausted family carers, stretched paid carers, the role of GPs, district nurses; it all feels very personal.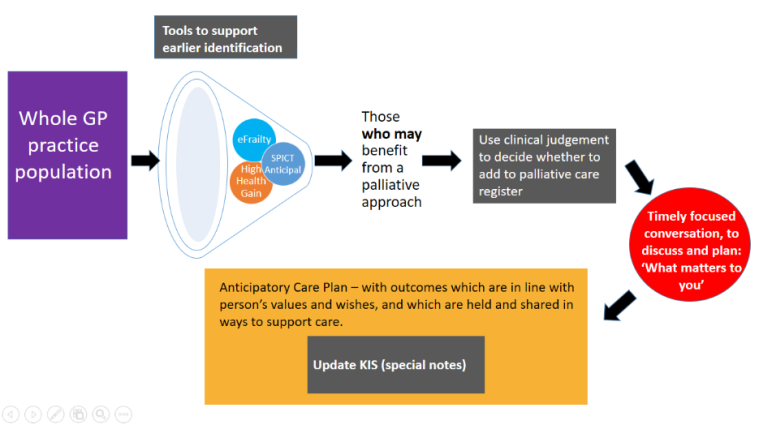

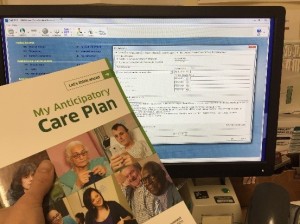 Anticipatory Care Planning is not a one-off event. It is a process that starts with a conversation and which can develop and evolve over time. The beauty of general practice is that we have opportunities to initiate that conversation and contribute to the development of an ACP over weeks, months and sometimes years.
Anticipatory Care Planning is not a one-off event. It is a process that starts with a conversation and which can develop and evolve over time. The beauty of general practice is that we have opportunities to initiate that conversation and contribute to the development of an ACP over weeks, months and sometimes years.
 sensitive conversations. Conversations should begin at the point of need by whoever is identifying the need / transition.
sensitive conversations. Conversations should begin at the point of need by whoever is identifying the need / transition.  Deans Buchanan (Consultant in Palliative Medicine, Lead Clinician) spoke about Health Transitions in Human Stories. Stories are very important to how we understand and communicate with one another. Most patients’ stories will have been interrupted by their illness and this can affect their response to treatment. The A, B, C, and D approach of dignity conserving care (Attitude, Behaviour, Compassion and Dialogue) is one method being tested to remind practitioners about the importance of caring for their patient.
Deans Buchanan (Consultant in Palliative Medicine, Lead Clinician) spoke about Health Transitions in Human Stories. Stories are very important to how we understand and communicate with one another. Most patients’ stories will have been interrupted by their illness and this can affect their response to treatment. The A, B, C, and D approach of dignity conserving care (Attitude, Behaviour, Compassion and Dialogue) is one method being tested to remind practitioners about the importance of caring for their patient.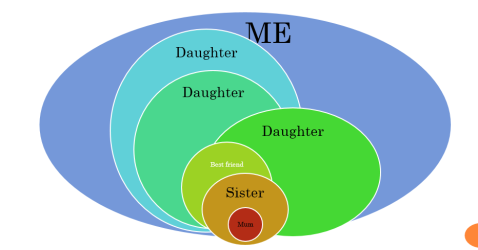
 ordination and Care Homes. As the population of over 80’s increases, they are becoming increasingly frail and more dependent, resulting in increased pressures on healthcare professionals supporting care homes. The main issues are:
ordination and Care Homes. As the population of over 80’s increases, they are becoming increasingly frail and more dependent, resulting in increased pressures on healthcare professionals supporting care homes. The main issues are: Richard Meade (Head of Policy and Public Affairs, Marie Curie Scotland) offered an insight in Looking Beyond 2021 and thinking about the future. As the population is living longer, more people will be diagnosed with multi-morbidities, including dementia, frailty and cancer, and will therefore require increased palliative care. This in turn will increase the pressures on every care setting, the workforce, resources and the way we deliver care, and we must act now.
Richard Meade (Head of Policy and Public Affairs, Marie Curie Scotland) offered an insight in Looking Beyond 2021 and thinking about the future. As the population is living longer, more people will be diagnosed with multi-morbidities, including dementia, frailty and cancer, and will therefore require increased palliative care. This in turn will increase the pressures on every care setting, the workforce, resources and the way we deliver care, and we must act now.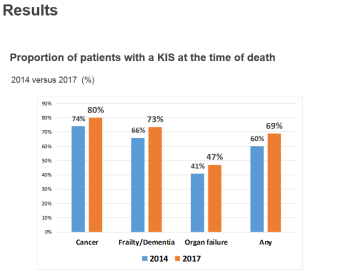 Information Summary (KIS) and a recent study undertaken on those who died with an advanced progressive condition in 2017 with a KIS in place. A KIS is a shared electronic clinical summary used to guide urgent care in the community and emergency hospital admission. It helps to communicate key elements and preferences from the person’s Anticipatory Care Plan (ACP) to help with future care needs.
Information Summary (KIS) and a recent study undertaken on those who died with an advanced progressive condition in 2017 with a KIS in place. A KIS is a shared electronic clinical summary used to guide urgent care in the community and emergency hospital admission. It helps to communicate key elements and preferences from the person’s Anticipatory Care Plan (ACP) to help with future care needs.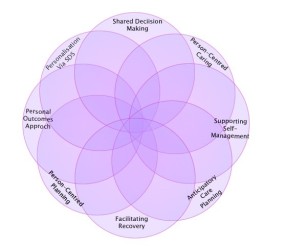 Ali Guthrie (Learning & Development Advisor) discussed Personal Outcomes: towards a Shared Understanding. A Personal outcomes approach is focusing on what is important to people in their lives. They often relate to maintaining or improving wellbeing and feature in the National Health and Wellbeing Outcomes in the new
Ali Guthrie (Learning & Development Advisor) discussed Personal Outcomes: towards a Shared Understanding. A Personal outcomes approach is focusing on what is important to people in their lives. They often relate to maintaining or improving wellbeing and feature in the National Health and Wellbeing Outcomes in the new