On 27 February 2020 we were joined by Away Team members from the 22 teams taking part in the Living and Dying Well with Frailty Collaborative. Teams travelled from across Scotland to come together for… More
Meet Paulo Nunes de Moura!
 Here’s a short introduction from Paulo Nunes de Moura, who has recently joined the Living Well in Communities team.
Here’s a short introduction from Paulo Nunes de Moura, who has recently joined the Living Well in Communities team.
I’m delighted to have joined the LWiC team as a project officer, and I’m focusing on the Living and Dying Well with Frailty Collaborative. I’m enjoying learning the work, and feel that I also have a lot to contribute because of my previous work experience, both paid and voluntary.
Previously, I worked as an events coordinator, being the lead organiser of the 8th European Alcohol Policy Conference, which took place at the Royal College of Physicians of Edinburgh. Other positions include working as a policy officer at the European Alcohol Policy Alliance, and in administrative posts at the University of Edinburgh.
I enjoy learning, and over the recent years I did complete Open University programmes for French and Spanish, completed a part-time master’s degree in Social Justice at Queen Margaret University, and graduated with a Bachelor of Laws from Robert Gordon University.
I also volunteered until recently at the Castlemilk Law Centre, where I completed detailed benefit application forms for clients living with complex physical and / or mental health conditions. This gave me an invaluable insight into the health issues that people face, as well as an appreciation for NHS online resources. I explored these with clients to identify information on conditions, as varied as schizophrenia, osteoarthritis and chronic obstructive pulmonary disease (COPD), with a view to gathering evidence to meet the necessary legal tests to access benefits.
Going off-topic a bit, another memorable experience from volunteering was meeting Queen Silvia of Sweden at a charity event in London, with whom I spoke briefly in Portuguese, as we are both Brazilian!
I’ve been enjoying working with many talented colleagues, who are very generous in sharing their great knowledge and enthusiasm about the fantastic work being done here. I’m also excited about having been given the opportunity to work with different professionals from organisations across Scotland. We are all focusing on improving people’s lives.
If you have any questions, then please do get in touch.
Getting ready for change

by Michelle Church, Improvement Advisor
‘Change matters. It forces us to act.’ – Will Storr
I started out writing this blog post like a report, out of habit. I want to develop a new writing style that is more appropriate for blogging, and it’s proving harder than I thought. This got me thinking, ‘Why is changing so challenging?’
A bit about habit…
I recently learnt that around half our waking day is habitual (see this study by Neal et al, which looks at experience-sampling diary studies), and that all of us have neurological loops that drive our behaviour. In Charles Duhigg’s, The Power of Habit, he explains that researchers at MIT discovered a simple neurological loop: cue, routine and reward.
They discovered that when designing new routines it is essential to identify the trigger for the action, otherwise old behaviours will continue. Also it turns out we don’t need to change the cue and reward for the change to stick. In fact, their research concluded not to: change only the routine. For new habits to form, we need to keep the same cue and reward.
Modes of thought
I have learned about how our brains are wired to be energy efficient. Daniel Kahneman, winner of the 2002 Nobel Memorial Prize in Economics, argues that we have two modes of thought: fast and slow.
The first mode of thought is fast. This is our natural state – automatic, intuitive, effortless. In this mode we create habits (patterns such as our route to work) to make living efficient. In the work environment these habits become the routines and processes that drive nearly every aspect of our working lives.
The second mode of thought is slow. It is deliberate, reflective and analytical. We go into this mode when planning a trip overseas, or learning something new.
When we experience change, when we learn or change a routine, we think more slowly and it takes effort. This may seem obvious, but it has transformed my ability to support improvement work. I have a greater understanding that the resistance to change is because we don’t like disrupting our habits – it goes against our energy-saving neuro-programming and reward structures.
There’s some good news, though, as it seems that we are also neuro-programmed for change. In The Science of Storytelling, Will Storr observes that we are alerted to things that might threaten our sense of control, becoming curious to discover the whole story and regain a sense of control. Our ability to be curious is a great starting point for improvement. Despite the effort required, most of us love to explore and learn.
Stepping outside of your comfort zone
If I’m honest, I normally want to explore a good castle or hillside and quickly return to my creature comforts. My experience of change that involves deep learning or changing my habits, where I am not sure what the change will involve and it seems beyond my control… well, it can often feel like the pits. James Nottingham sums it up well in his visual journey of the learning challenge. He uses the image of a pit to illustrate the obstacles that people encounter in learning something new, and how it takes them out of their comfort zone.

Source: Challenging Learning
Combining John Fisher’s Personal Transition Curve with this image of the learning journey can help us to understand how individuals might respond to change, and consider what might move people into acceptance and take up new behaviours.
In addition to understanding the challenges associated with learning something new, it is also important to consider what motivates people. Daniel Pink (author of Drive, which explores human motivation) argues that intrinsic reward, doing something because we find it gratifying, is as just as important as biological and extrinsic rewards.
Discovering the personal and relational, intrinsic and extrinsic motivations is essential to understand the reward we all need.
Breaking habits
Change is challenging, as habit is such a dominant force in our lives. However, understanding the reasons why we find it difficult to change, tapping into people’s curiosity and desire to learn, and understanding their motivations can help us to break away from old habits, and create new ones.
Sharing knowledge through podcasts

by Laura Dobie, Knowledge and Information Skills Specialist
Dr Calvin Lightbody is a consultant in Emergency Medicine at NHS Lanarkshire, and he also produces the Talking Mortality podcast. He recently recorded an episode with our clinical lead for palliative and end of life care, Dr Paul Baughan, on supporting people with frailty in the community.
Everybody’s talking about podcasts…
Podcasts are becoming increasingly popular, and are available on a variety of platforms, which makes them very easy to access. They cover a wealth of subjects, and the format lends itself equally to presenting bite-sized chunks of information, to more in-depth exploration of a topic.
There is a podcast for everyone, whatever their interests or time commitment. This growing appetite for audio is also reflected in audiobook sales, which are growing as sales of print books are falling.
Getting into it
Calvin has 20 years of healthcare experience, and has recently been working to improve the care that hospital patients receive towards the end of life. He decided to give podcasting a try after putting a lot of time and effort into preparing and promoting a presentation at an event, which was not as well-attended as he had hoped. This prompted him to consider how he could reach more people, and he thought that podcasts could be the ideal medium.
Why podcasts?
Podcasts have numerous benefits. You can listen to them anywhere, at any time. They have multitasking potential: people can listen to them while doing other things, allowing them to take in information on their commute, while hanging up the washing, or cooking. They also cater to expectations for on-demand content: Calvin observed that people do not tend to watch live TV as much as they used to, and are increasingly shifting to streaming services to watch what they want, when they want.
Podcasts provide people with information and entertainment, in a format that fits around their busy lives. They also have considerable potential for learning and development: Calvin listens to a lot of medical podcasts that contribute to his CPD.
The Talking Mortality podcast
Talking Mortality explores the difficulties and challenges of human mortality. Individuals, society in general and health and care professionals all struggle with this issue. The podcast aims to start conversations on this topic. Previous episodes have covered areas such as dementia, palliative care, anticipatory care planning, and the death taboo.
 Calvin’s recording studio for the day was Dollar Health Centre, where Paul works as a GP. His set up is fairly minimal: a USB microphone plugged into laptop to record the audio, and headphones to check the sound. The podcast format is an intro from Calvin, an interview with his guest speaker, and a recap of key learning from the podcast at the end. This really reinforces potential of the podcast for sharing knowledge and getting it into practice.
Calvin’s recording studio for the day was Dollar Health Centre, where Paul works as a GP. His set up is fairly minimal: a USB microphone plugged into laptop to record the audio, and headphones to check the sound. The podcast format is an intro from Calvin, an interview with his guest speaker, and a recap of key learning from the podcast at the end. This really reinforces potential of the podcast for sharing knowledge and getting it into practice.
The recording with Paul is seamless. Calvin records a brief intro to check the sound, then they go straight into a conversation, which is recorded in one take. Half an hour flies by, taking in the importance of identifying people with frailty, what GP practices can do to support people with frailty, and anticipatory care planning, amongst other topics.
After editing, Calvin adds the podcast to Buzzsprout, a podcast hosting site. You can listen to Paul’s episode now, and access all the earlier episodes.
Want to continue listening?
There is a wealth of health and social care podcasts within easy reach of your headphones. Here are a few to get you started:
- MDTea podcast – A series of podcasts aimed at healthcare professionals working with older adults.
- Nice Talks – Individual stories behind NICE’s work to improve care through evidence-based guidelines.
- Iriss fm – Research, projects and events on topics related to social work and social care.
- GEMCAST – A geriatric emergency medicine podcast aimed at clinicians, nurses, or paramedics who take care of older adults, particularly in the Emergency Department.
Do you listen to podcasts? What are your favourite podcasts that cover health and social care?
Meet Sarah O’Shaughnessy!

Sarah O’Shaughnessy, one of the project officers in our team, talks about her role and what she enjoys about the job. It’s all about the people!
I started working with the Living Well in Communities (LWiC) team at the end of July, having been project officer with the Mental Health Improvement Team in the six months before that. I have been working at Healthcare Improvement Scotland (HIS) for two and a half years.
The thing that I really enjoy about my job is working with people. Some of my favourite experiences since starting with the LWiC Team five months ago have been engaging with stakeholders. This might be in person or over the phone, discussing how they can put their skills together and achieve the goal of improving the lives of people in Scotland.
At the moment one of my main pieces of work if the Living and Dying Well with Frailty Collaborative. I am responsible for supporting my colleagues and the teams in the west. I am gradually getting to know the teams and really enjoy the opportunities I get to speak with team members more. From my point of view, the better I know the teams, the better I can support them. What I like to know is how people like to be communicated with? Do they prefer a phone call or an email, do they like reminders, do they use Twitter, how do they find using the Knowledge Hub? If you are one of the people in these teams, please feel free to get in touch and let me know how I can communicate with you more effectively!
I have recently started working with some of my colleagues on our anticipatory care planning (ACP) documentation. This has been quite a steep learning curve for me, but it has been fascinating. I am particularly enjoying seeing how ACP can be used to support work across Health and Social Care Partnerships, and we have had some invaluable feedback on how it is currently being used and how it could be used better in future.
While I am finding both projects interesting, the thing that I am really enjoying is the people. The passion and the knowledge of the people I work with, both within and outside of HIS, never ceases to amaze me. In the last few months I have learned so much because of people around me and the opportunities that I have been given.
My hope is that my learning will continue and that people will continue to let me engage with them. I would love to hear back from people about what interests them about the work they do, if you are someone I engage with, let me know how I can do this better too! If you are on Twitter my handle is @SarahOShaughne3 Feel free to follow me, especially if you like the occasional update on the Glasgow Warriors!
Mr Lucas’ Story
Dr Paul Baughan, our National Clinical Lead for Palliative and End of Life Care and GP in Dollar, tells us about Mr Lucas who appears in our new video below.
My first contact with Mr Lucas was sadly not a pleasant one. It was Christmas Eve 2014 and he had travelled from Birmingham to spend time with his family. I was called when he suddenly took unwell, and I sent him to hospital for treatment of an evolving stroke. Mr Lucas spent that Christmas in hospital.
Stroke disease is one of many conditions which contribute to ‘frailty’. People living with frailty have reduced resilience to illnesses such as infections, to injuries following falls, or to emotional stress such as following a loss or bereavement. This makes people living with frailty particularly vulnerable and at risk of unplanned admission to hospital.
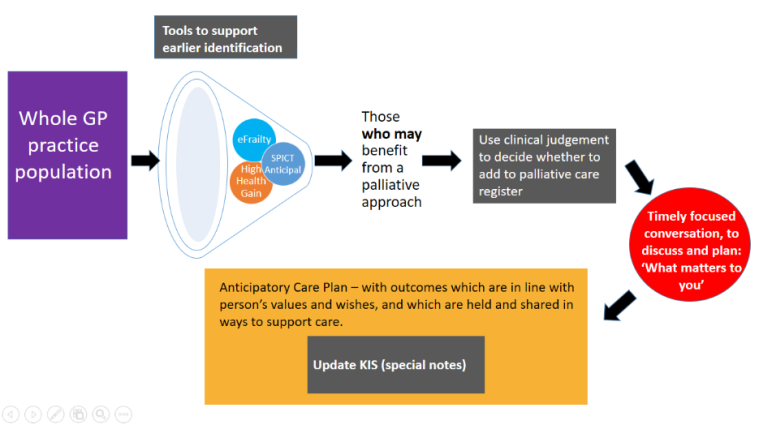
However by identifying people living with frailty at an earlier stage through tools such as the eFI (electronic frailty index), it is possible to provide evidence-based interventions and support which can help them live independently at home. At the moment 21 teams across Scotland are taking part in the Living and Dying Well with Frailty Collaborative to improve the care provided to people with frailty. These teams are looking at how health and social care can work more closely together to support people as they become more frail.
By identifying people early, before a crisis, and putting in the right services and support, it is possible to help those with frailty to live a fulfilling life in their own homes.
Mr Lucas moved to live in Clackmannanshire following his stroke so that he could be closer to his family. In this video Mr Lucas gives a clear account of how he is supported to enjoy the things that are important to him – his books and good music. He describes how aids and equipment around his house have helped him, and the huge impact that professional carers make to his day to day life. I first met Mr Lucas in difficult circumstances. It was a delight to interview him for this video and to see how his life has changed and been enhanced through this vital support.
Living and Dying Well with Frailty Collaborative – Learning Session One

On 19 September 2019, 21 teams taking part in the Living and Dying Well with Frailty Collaborative came together for the first learning session where they learned how to test their ideas using a range of improvement methods, and how to measure their activities and the impact they make. They also heard from each other about the frailty work being undertaken in the various Health and Social Care Partnerships and GP practices, and had time as a team to look at their project charter and develop their plans for their next test of change during the learning session action period.
Living with Frailty
People are at the heart of what we do, so we started the day by hearing from those living with frailty. We heard about the experience of Mr Lucas, who featured in our video. He spoke about how the support that he receives from services and family helps him to live independently with frailty. Mr Lucas is one of Dr Paul Baughan’s patients, the Living Well in Communities (LWiC) National Clinical Lead for Palliative and End of Life Care and GP at Dollar Health Centre.
 “I hope I’m as able as Mr Lucas when I have moderate frailty. I love how it was the carers, reading and music that helped him live well with frailty.”
“I hope I’m as able as Mr Lucas when I have moderate frailty. I love how it was the carers, reading and music that helped him live well with frailty.”
We also had Hugh Donaghy join us for the day. Mr Donaghy is a carer for his mother and spoke to Professor Graham Ellis, the LWiC National Clinical Lead for Older People and Frailty, about his experience of providing care to someone living with frailty. Hugh discussed how technology is helping him to support his mother in her home, the blurred line between being a carer and a relative, and the challenges of hospital stays: each time his mother comes out of hospital, her frailty increases.

“Carer experience of mum with long term conditions going in to hospital ‘each time she comes home she’s that bit frailer’ – how can we build resilience when someone comes back home?”

I want to be involved in the Frailty Collaborative because…
Alec Murray, Associate Improvement Advisor, led a short ice breaker with the teams using Slido to ask the teams how they felt about being involved in the collaborative, creating the word cloud below…

It was great to see people and care at the centre.
Throughout the day there were a number of questions asked on Slido. We didn’t have the opportunity to respond to all of these on the day, so we’ve pulled together our answers in this form: Slido Questions and Answers
Learning about Improvement
The teams then had the opportunity to learn about Quality Improvement Methods and Measurement for Improvement, led by the Living Well in Communities Improvement Advisors and Associate Improvement Advisors (Nathan Devereux, Scott Purdie, Dianne Foster, Tom McCarthy and Michelle Church).
Quality Improvement Methods
When we designed this session we wanted to explore with the teams a range of Quality Improvement concepts and tools. We held an introductory WebEx where we polled the teams to find out how much knowledge and experience everyone had in using QI tools. The teams told us that there was a real mix of skills and experiences in the room, and the results indicated that we should spend a little bit more time on the change package. Therefore the session was designed to give everyone a flavour of some of the approaches that might help teams in the action period.
At the end of the session, the teams were asked for their lightbulb moments:
“Build on existing practice and evidence with data”
“Small steps to improvement are better than a leap of faith”
“Even failed attempts are learning and a critical part of improvement”
“Don’t reinvent the wheel – SHARE”
“In order to spread change, you need to explain to others why it’s important, how it works and have a narrative”
Measurement for Improvement
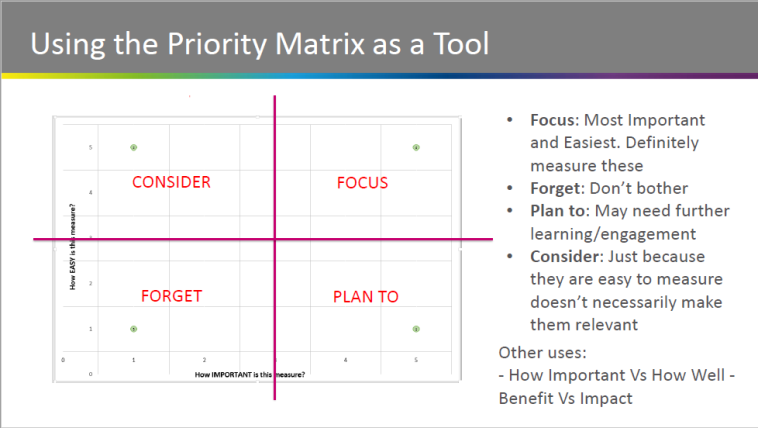
As this was the first session we aimed to get everyone on the same level, so that teams were prepared for the first action period. We covered some of the practical elements of measurement for this collaborative, including the data collection method.
The collaborative is focused on three core measures, which represent an increase in involving people in conversations about their needs and care, and also a shift to more planned activity.
In the session we introduced the measurement plan tool designed to help teams collect this data and also provided time for teams to consider what their measurement priorities are, including local priorities and measures which take account of interventions (such as polypharmacy).
It was great to discuss measurement of the collaborative at the first learning session and particularly to hear the views of teams about how best to approach what can be one of the trickiest parts of improvement – measuring whether you make a difference.
Learning from Across Scotland
We had 15 teams and national organisation representatives host tables where they presented on what work they have undertaken on frailty in their area. This was ‘world café’ style, where everyone had an opportunity to go to three tables and hear about work in other areas and ask questions.
There were some great discussions, and the feedback we received indicated this was a very popular session. It was beneficial for them to hear about what is happening in other areas and have the chance to discuss challenges faced, as well as successes.
For example, Rebecca McLaren and Eileen Downham from the Angus team presented work on their Enhanced Community Service and community multidisciplinary team (MDT) meetings. The challenge faced in Angus is that a person can be registered to any of eight GP practices because practice boundaries overlap. The group were particularly interested that a medicine for the elderly consultant from hospital attends the community MDT meetings. If a consultant can’t attend then an advanced nurse practitioner attends in their place.
North Lanarkshire HSCP has been working with hospital at home and 30 GP practices to test MDTs. They found the challenges were around data and how home visits can be recorded. Also whether it is possible to measure the quality of ACPs, and creating an infrastructure to support people wishing to stay at home.
For a full list of these topics please click here. For more information about anything which was discussed, please get in touch via email – hcis.livingwell@nhs.net – and we can put you in touch with the relevant team.
Team planning
Teams were then given time to work together on their project charter and action planning for the first action period of the collaborative.

If you are undertaking similar improvement work you may find the below resources helpful:
 “Fantastic reasons to be at #LWiCFrailty today. But “a goal without a plan is just a wish” so now time for action! Thanks for a useful day of sharing & learning @LWiC_QI @eFI_Midlothian”
“Fantastic reasons to be at #LWiCFrailty today. But “a goal without a plan is just a wish” so now time for action! Thanks for a useful day of sharing & learning @LWiC_QI @eFI_Midlothian”
What next?
Away teams will share their learning with the Home Teams and begin their tests of change, or continue with any tests already underway. They will be documenting their progress and recording data over time, with the support of the Improvement Advisors and Associate Improvement Advisors who are area leads for each of the teams.
For more information about the collaborative please visit https://ihub.scot/improvement-programmes/living-well-in-communities/our-programmes/living-and-dying-well-with-frailty/
For the PowerPoint slides from the day from all sessions, please click here.
What works in care co-ordination in palliative and end of life care
 We have recently published a resource that reviews the evidence on continuity and care coordination in palliative and end of life care. This blog post gives an overview of the document and its features.
We have recently published a resource that reviews the evidence on continuity and care coordination in palliative and end of life care. This blog post gives an overview of the document and its features.
Why focus on care coordination?
Good care co-ordination can help to improve people’s quality of life, right up to the end of life.
The Living Well in Communities team has been working with test sites in Dundee, East Ayrshire, Fife, Glasgow City, and Renfrewshire Health and Social Care Partnerships to deliver Commitment 1 from the Scottish Government’s Strategic Framework for Action on Palliative and End of Life Care:
“We will support Healthcare Improvement Scotland in providing Health and Social Care Partnerships with expertise in testing and implementing improvements to identify those who can benefit from palliative and end of life care and in the co-ordination of their care.”
This work is coming to a close in March 2019.
Exploring the evidence on different approaches
Drawing on the priority practices outlined in the World Health Organization practice brief on continuity and co-ordination of care, we identified six key approaches to continuity and care co-ordination in palliative and end of life care:
- Early integrated palliative care
- Collaborative planning of care and shared decision making
- Case management for people with palliative and end of life care needs
- Intermediate palliative care at home
- Technology to support continuity and care coordination
- Building workforce capacity
Working with the Evidence and Evaluation for Improvement Team, we summarised the available systematic-review level evidence on these approaches.
Presenting the evidence visually
As with our Living Well in Communities with Frailty evidence review, we produced visual summaries for each of the approaches. These provide key information on the different approaches to care coordination, and an introduction to the more detailed evidence summaries. The visual summaries include
- a brief description of each approach,
- the rationale behind them,
- the potential benefits,
- enablers,
- brief commentary on the quality of the evidence, and
- links to further reading and examples of local good practice.
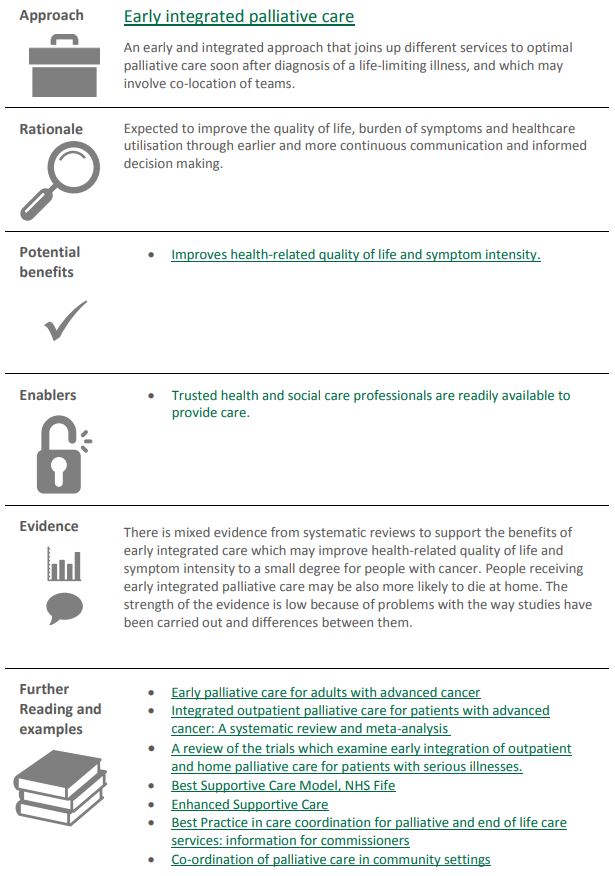
We hope that this document will provide a useful overview of the systematic review-level evidence on key approaches to care co-ordination in palliative and end of life care, and highlight the potential benefits of these approaches.
You can access the review, Continuity and Co-ordination in Palliative and End of Life Care: evidence for what works by clicking on the document image below:
Care Co-ordination Short Stories
A number of Palliative Care professionals who attended our Palliative and End of Life Care Delivery Group on 8th November kindly shared some insights into how to better understand care co-ordination. You can find out more by looking at the slides from the day here.
Sandra Campbell (National Clinical Lead) presented on the importance of timely,  sensitive conversations. Conversations should begin at the point of need by whoever is identifying the need / transition. The Palliative Care Identification Tools Comparator can be used to allow people to make more informed choices about their care and treatments when they have an irreversible illness. Significant conversations happen at the right time, in the right place with the right person.
sensitive conversations. Conversations should begin at the point of need by whoever is identifying the need / transition. The Palliative Care Identification Tools Comparator can be used to allow people to make more informed choices about their care and treatments when they have an irreversible illness. Significant conversations happen at the right time, in the right place with the right person.
 Deans Buchanan (Consultant in Palliative Medicine, Lead Clinician) spoke about Health Transitions in Human Stories. Stories are very important to how we understand and communicate with one another. Most patients’ stories will have been interrupted by their illness and this can affect their response to treatment. The A, B, C, and D approach of dignity conserving care (Attitude, Behaviour, Compassion and Dialogue) is one method being tested to remind practitioners about the importance of caring for their patient.
Deans Buchanan (Consultant in Palliative Medicine, Lead Clinician) spoke about Health Transitions in Human Stories. Stories are very important to how we understand and communicate with one another. Most patients’ stories will have been interrupted by their illness and this can affect their response to treatment. The A, B, C, and D approach of dignity conserving care (Attitude, Behaviour, Compassion and Dialogue) is one method being tested to remind practitioners about the importance of caring for their patient.
Heather Edwards (Dementia Consultant, Care Inspectorate) gave a good overview of Bereavement. Heather highlighted the importance of preparation for death and the value of the care home staff in supporting families. Bereavement can cause an emotional toll on the staff as well as families but it’s important that we also support them as they are also grieving having developed relationships with the residents and their families.
Lynne Carmichael (Respite & Response Team Manager, Ayrshire Hospice) presented on carers and the Carers Support Needs Assessment Tool (CSNAT). One of the first barriers is many carers do not recognise themselves as a carer and often put their own needs to the side to care for a loved one. The CSNAT tool helps provide support for family members and carers of those with a life limiting condition.
Jo Hockley (RN PhD, Usher Institute, University of Edinburgh) presented on Care Co- ordination and Care Homes. As the population of over 80’s increases, they are becoming increasingly frail and more dependent, resulting in increased pressures on healthcare professionals supporting care homes. The main issues are:
ordination and Care Homes. As the population of over 80’s increases, they are becoming increasingly frail and more dependent, resulting in increased pressures on healthcare professionals supporting care homes. The main issues are:
– Lack of recognising the dying
– Lack of healthcare support to palliative care
– Lack of support staff
More work will need to be done around linking care homes into the system. This will hopefully be aided by a similar study to the Teaching Nursing Home pilot whereby the public/professional perception of care homes change, encouraging a career pathway in care homes for health and social care professionals, to help increase the workforce and establish more community engagement in care of frail older people.
 Richard Meade (Head of Policy and Public Affairs, Marie Curie Scotland) offered an insight in Looking Beyond 2021 and thinking about the future. As the population is living longer, more people will be diagnosed with multi-morbidities, including dementia, frailty and cancer, and will therefore require increased palliative care. This in turn will increase the pressures on every care setting, the workforce, resources and the way we deliver care, and we must act now.
Richard Meade (Head of Policy and Public Affairs, Marie Curie Scotland) offered an insight in Looking Beyond 2021 and thinking about the future. As the population is living longer, more people will be diagnosed with multi-morbidities, including dementia, frailty and cancer, and will therefore require increased palliative care. This in turn will increase the pressures on every care setting, the workforce, resources and the way we deliver care, and we must act now.
Anne Finnucane (Research Lead, Marie Curie Hospice Edinburgh) presented on the Key 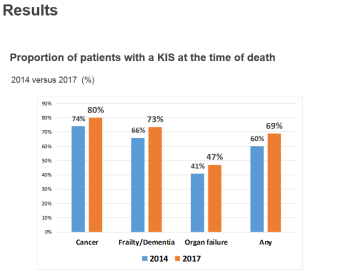 Information Summary (KIS) and a recent study undertaken on those who died with an advanced progressive condition in 2017 with a KIS in place. A KIS is a shared electronic clinical summary used to guide urgent care in the community and emergency hospital admission. It helps to communicate key elements and preferences from the person’s Anticipatory Care Plan (ACP) to help with future care needs.
Information Summary (KIS) and a recent study undertaken on those who died with an advanced progressive condition in 2017 with a KIS in place. A KIS is a shared electronic clinical summary used to guide urgent care in the community and emergency hospital admission. It helps to communicate key elements and preferences from the person’s Anticipatory Care Plan (ACP) to help with future care needs.
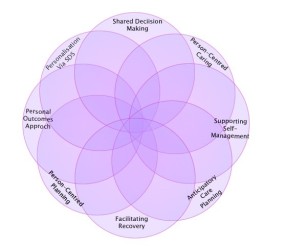 Ali Guthrie (Learning & Development Advisor) discussed Personal Outcomes: towards a Shared Understanding. A Personal outcomes approach is focusing on what is important to people in their lives. They often relate to maintaining or improving wellbeing and feature in the National Health and Wellbeing Outcomes in the new Health and Social Care Standards.
Ali Guthrie (Learning & Development Advisor) discussed Personal Outcomes: towards a Shared Understanding. A Personal outcomes approach is focusing on what is important to people in their lives. They often relate to maintaining or improving wellbeing and feature in the National Health and Wellbeing Outcomes in the new Health and Social Care Standards.
For further information, please contact a member of our team at hcis.livingwell@nhs.net
Follow us on Twitter:@LWIC_QI, @turnersara99 @paulbaughan, @sandracampbellc65402031
Neighbourhood Care Steering Group, 3rd October – Challenges and Support
On the 3rd October we held our latest Neighbourhood Care Steering Group at the Edinburgh Training & Conference Venue. There was great representation from the Neighbourhood Care test sites [including Western Isles, NHS Highland, Aberdeen City, Scottish Borders, Stirling & Clacks and Cornerstone] as well as national supportive partners [Scottish Government, Buurtzorg Britain & Ireland, SSSC, Care Inspectorate and NES].
The aim of the day was to openly discuss the challenges and support that National Partners and test sites can offer each other.

Defining our Measures
Thomas Monaghan (HIS) and Fee Hodgkiss (Scottish Government) revisited the vision set out in 2016 for Neighbourhood Care, in a letter from Scottish Government. Both discussed whether the principles are still relevant today, and what they mean in a Scottish context. They offered the opinion that as a set of principles, they were solid and aligned with the pillars of providing person-centred, ‘good, old-fashioned’ care. The group agreed that the principles still applied in a Scottish context and there was a general consensus that the principle of person-centred care was most important.
Logic Model-Measurement Mapping
The group were led through a cross mapping exercise carried out by the ihub team that links the original desired outcomes and impact of the programme’s logic model with the current measures being undertaken in local test sites.
The measures were themed into six categories:
- Re-ablement
- Person satisfaction/experience
- Staff satisfaction
- Procedural tasks
- Workforce structure
- Professional autonomy/self-management
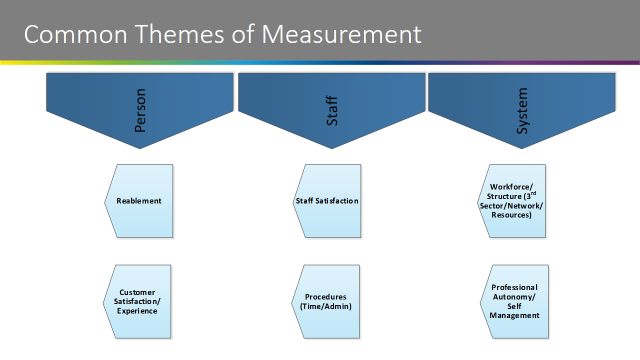
The exercise highlighted that there may be areas of measurement that were not currently being recorded. Key to this part of the morning was to facilitate agreement on potential measures for Neighbourhood Care Teams at a national level, and the group discussed this and what measures could potentially ‘fill the gaps’ if necessary.
There was consensus within the group that the themes were good. The group also highlighted the need for “Third Sector/communities capacity building contribution” to be added as a 7th theme for measurement.
The group agreed that further discussion focussing on the measures within the document would be of benefit, and a small sub-group will be formed to carry this out. This group will meet and develop a set of common measures for all sites based on these (now seven) highlighted themes before the next steering group in November. If you have any suggestions, please get in touch with your local lead or contact hcis.livingwell@nhs.net
Challenges and Support
The group was asked to reflect on the nine common themes of challenges that sites were reporting and were asked to consider opportunities for peer support and/or offers of support from national partners.
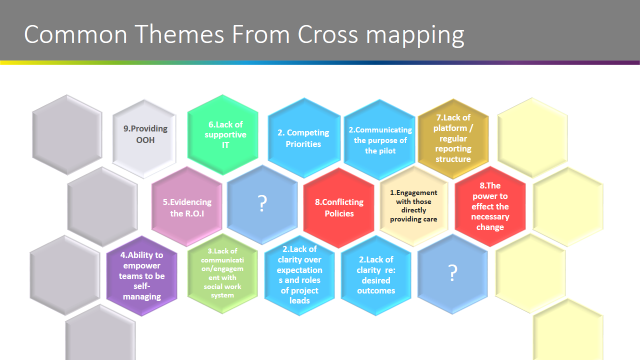
The group selected three themes and spent the remainder of the afternoon discussing these:
Number 4: Ability to empower teams to be self-managing
Number 2: Competing Priorities and Communicating
Number 7: Lack of platform / regular reporting structure
“Self-organising” came up as a key challenge being faced by the test sites. The group agreed there is potential for some rich learning that could be shared from Buurtzorg Britain and Ireland and Cornerstone’s approach and experience with this.
HIS will work alongside Britain Buurtzorg and Ireland and Cornerstone to develop a series of recorded WebExes that will provide further information on this (and other fundamental topics) and will share these on our website. Watch out for a programme of dates for these, which we’ll communicate soon.
Care Experience Tool
In order to support sites to measure ‘experience’ (versus satisfaction) a Care Experience Tool (developed in collaboration between the LWiC and Evidence and Indicators team within HIS) was shared in a draft form. The tool is a set of open questions that aim to explore compassionate care, and are directly related to the new Health and Social Care Standards. Aberdeen City, Stirling and Clackmannanshire and Cornerstone were interested in testing out the tool. It’s great that our public partners have agreed to support sites with this work.
The group also discussed the practical use of the tool and further training and development dates will be planned.
Having a platform for regular sharing/reporting
The Steering Group expressed that having the opportunity to meet, chat and share ideas, knowledge and offers of support is always extremely valuable. Steering groups only happen every 6-8 weeks, so the LWiC team agreed to set up a webpage for the group on the Knowledge Hub. This will be a platform for sites to share information around Neighbourhood Care in between meetings and will be open to all roles in all areas. We look forward to sharing more details around this in the future.
For any further information on any of the above, please feel free to contact one of the team:
The community-based interventions that can make a difference for people with frailty

We have recently published a resource that summarises the evidence for different community-based frailty interventions. This blog post gives an overview of the document and its features.
Why focus on frailty?
A person with frailty can experience serious adverse consequences following even a relatively minor illness. Its impact can be very significant in terms of consequent disability or admission to a nursing home.
If frailty is identified at an early stage and individuals are targeted with evidence-based interventions that can manage frailty, or reverse it, this can improve people’s quality of life and wellbeing. This reduces the likelihood that they will need to access unplanned services due to a crisis, which, in turn, reduces the use of expensive, unscheduled care.
The community-based interventions that can make a difference
The literature on frailty is vast. For the purposes of our resource we focused on interventions in frailty that are community-based, focused on the prevention of harms or poor outcomes, and supported by relatively high-level evidence. The Evidence and Evaluation for Improvement Team carried out literature searches and produced evidence summaries for the following topics:
- Exercise interventions and physical activity
- Polypharmacy review
- Immunisation
- Primary care interventions
- Community geriatric services
- Lifestyle factors: physical activity diet, obesity, smoking alcohol and their relation to frailty
- Nutritional interventions for the prevention and treatment of frailty
- Hospital at home: admission prevention and early discharge
- Reablement (including rehabilitation)
- Bed-based intermediate care
- Anticipatory care planning
Making the evidence accessible
We then created visual abstracts for each topic, which allow readers to compare the different interventions at a glance, and provide a route into the more detailed evidence summaries and further reading. The visual abstracts include information on the potential benefits of each intervention, evidence quality, costs, and frailty level:


We hope that this document will help Health and Social Care Partnerships to compare different interventions for frailty and the evidence behind them, and to consider which interventions could make a difference for people with frailty in their local areas.
You can access the report, Living Well in Communities with Frailty: evidence for what works by clicking on the document image below:
Palliative and End of Life Care: Focus on Identification
Michelle Church, Improvement Advisor, reflects on our recent learning event, which explored ways of identifying people who could benefit from a palliative approach to their care.
On 31st May 2018, test site participants from six health and social care partnerships (HSCPs) and key delivery partners across Scotland joined the Living Well in Communities team to learn and share knowledge about tools that can support identification of people who could benefit from a palliative approach to their care.
Making the case for early identification
Kirsty Boyd, consultant and lecturer in Palliative Medicine, talked about the many benefits of earlier identification:
- Helps people say what matters to them.
- Increases the opportunity for people to participate in decision-making.
- Reduces the risk of later regrets and poor outcomes.
- Gives people time for planning ahead, resulting in fewer crises.
- Reduces unplanned admissions of low benefit.
- Encourages medication review and treatment planning.
- Improves continuity and coordination of care by sharing information.
How can we do earlier identification?
Our national clinical leads, Dr Paul Baughan and Sandra Campbell, gave an overview of the visual resource the LWiC team have developed to help compare different identification tools that are currently used in Scotland. Sandra did a before and after survey of how aware and confident participants were about the variety of tools.
How did we mobilise knowledge?
Experts from across the UK shared their tools, knowledge and experience of doing identification. People got the chance to participate in interactive workshops looking at the tools that a number of palliative care test sites. Some insights from the sessions are included below:
Anticipal and eFI electronic tools
SPICT4ALL and carers identification
What did people think of the event?
People felt that they had learnt about why, when and how to use different tools to support identification and inform practice. People really liked that they had the chance to network with experts and colleagues.
Overwhelmingly, the take home message was that earlier identification and communication is key to supporting those who would benefit from a palliative approach to their care.


What next?
HSCP palliative care test sites are now using the comparator to consider what tools will benefit local people and services and how people identified can be supported. This work will contribute to the vision that by 2021 everyone who could benefit from palliative care will have access to it and will support the Realistic Medicine ambition of shared decision-making and a personalised approach to care.
Reflecting on our palliative care work: thoughts from Paul Baughan
 Dr Paul Baughan, our palliative care GP clinical lead, discusses the benefits of early palliative care, highlights a resource that we’ve developed to compare different palliative care identification tools, and looks ahead to future work on care planning and care coordination.
Dr Paul Baughan, our palliative care GP clinical lead, discusses the benefits of early palliative care, highlights a resource that we’ve developed to compare different palliative care identification tools, and looks ahead to future work on care planning and care coordination.
Having worked within General Practice for over 20 years, I have seen the transition from hospital-based care to community care for a wide variety of clinical conditions and diseases. We look after many more people who are living with complex medical diagnoses well into their 80s, 90s and beyond. It can be difficult to identify when a palliative approach to care should be considered, and as a result we sometimes find ourselves on the back-foot, reacting to events and changes in clinical condition. Often, with the benefit of hindsight, it might have been possible to anticipate and plan for these episodes before they happen.
This is one of the reasons that I have enjoyed the opportunity to work with Healthcare Improvement Scotland and five test sites across Scotland (Dundee, East Ayrshire, Fife, Glasgow, and Perth and Kinross) to explore how we might identify people who could benefit from a palliative approach to their care at a much earlier stage.
Although a variety of different electronic and paper ‘tools’ have been developed by academics to help identify those who might benefit from a palliative approach to their care, it can be confusing to know which tool to use, and in which situation. Some are electronic, some are designed for particular diseases such as cancer or dementia, or for particular settings such as care homes. Some tools are intended for health professionals and some for the general population. I have therefore enjoyed working with the team in Healthcare Improvement Scotland to design a resource which will help health and social care professionals become more familiar with the different identification tools, and most importantly, decide which one suits them best. Our five test sites have chosen different identification tools to use within their local Health and Social Care Partnerships.
However, identifying those who might benefit from a palliative approach to their care is just the first step. It is the conversations that follow, between the health and social care professionals and the person, that are important. And then of course the care planning that results from these discussions. This is our next area of focus at Healthcare Improvement Scotland. We are now working with our test sites to explore how best to plan, coordinate and deliver care to those who are living with a progressive life-limiting condition.
This is an exciting phase of our work, as each test site is considering innovative and practical ways to provide this care within existing resources, and across health and social care. We will have the opportunity to share some of the learning from across Scotland in the Autumn, with the full outcomes from our test site projects available in 2019.
Back at my own general practice, my colleagues and I will continue to see an increase in the number of people with complex progressive life-limiting conditions in the years ahead. Therefore, the outcomes from the five test sites will be very relevant to the work that we do on a daily basis. We know that a proactive, multi-professional, care planning approach is required, and eagerly await advice from the test sites regarding how best to achieve this.
Highlights from the Neighbourhood Care Learning Network Event
On 11 May 2018 we held our latest neighbourhood care learning network event at the Care Inspectorate Offices in Hamilton. The session was well -attended by representatives from the neighbourhood care test sites, national organisations and third sector organisations. The purpose of this meeting was to discuss neighbourhood care and regulation, with a focus on questions raised by the test sites before the meeting. We also took the opportunity to discuss measurement ideas and learn what plans were already in place for local evaluation.
Sharing learning from the test sites
After introductions, staff from each test site provided an update on the neighbourhood care work in their area. There has been a lot of activity across the test sites with positives discussed on this way of working, offers of support and an eagerness from sites to arrange visits to learn from one another. Common challenges faced by the sites include those around culture and shifting perceptions, but the passion for the concept and success stories continue to drive this work forwards and motivate the teams.
Care Inspectorate – from enforcers to enablers
Catherine Agnew from the Care Inspectorate gave an informative presentation about the role of the Care Inspectorate in supporting services as enablers of innovation, rather than the traditional perception of enforcing regulation. There is acknowledgement that services for the public are evolving with the integration of health and social care. In support of this, the Care Inspectorate have developed regulatory sandboxes, where normal regulatory requirements are waived to support innovation which has the potential for public benefit.
Attendees discussed the new health and social care standards in Scotland and were pleased to note that the principles of the Buurtzorg model mirror these standards (Dignity and respect; Compassion; Be included; Responsive care and support; Wellbeing).
Evaluation
We facilitated a group discussion on evaluation and undertook an exercise to look at measures, how important these are and how easy they are to use. Representatives from the test sites rated examples and entered them into a prioritisation tool, which could help the teams to look at work priorities and measurements in their areas. They highlighted difficulties with measuring face-to-face contact time, although this is an important measure to show effectiveness of this model and the test site representatives acknowledged that this is a measure that is important to care givers: ‘more time with the person needing care’.
They are aware that while test sites will have different measures and there will be local variation, there is a need to have some standardisation for comparisons. Evaluation should be meaningful in a local context for individuals, their carers and staff. However, an element of evaluation will be required for national interest to look at areas such as cost saving, avoiding hospital admissions and reducing length of stays, etc.
The King’s Fund has recently published a paper on transformational change in health and care in response to the growing pressures and demands on the health and care system. The paper highlights four case studies that have been recognised as successful transformation initiatives, led by staff that directly provide care and service users. One of these successful initiatives is the Buurtzorg Nederland model.
Next steps
The test site representatives agreed to try a new approach to the learning network, with an option to move to the IHI model of a breakthrough series collaborative alongside action learning sets facilitated by the Scottish Social Services Council in the future. Once logistics have been further discussed, options will be presented to the group to take forward. Members of the group were happy to share their plans for evaluation with the Living Well in Communities (LWiC) team and there are steps to visit each site. Further information will be available soon.
Introducing Maxine Jones

I’ve had a long career in generalist primary care practice management, so stepping into a new role as Fife’s palliative care improvement advisor may have seemed at first like a leap into unfamiliar, specialist territory.
But, as one doctor said to me, palliative care is the bread and butter of primary care.
Both services share a deep-rooted holistic philosophy that deals with the emotional, social, practical and spiritual aspects of health and well-being, as well as the medical management of illness.
So, for me, a move to palliative care felt like a home coming.
Improvement work
I’m working with Fife’s health and social care partnership to realise the Scottish Government’s vision, that by 2021 everyone who needs palliative care will have access to it.
Our aim is to innovate and improve the identification and care coordination for people who may benefit from palliative care.
What people want is support to live well, safely and for longer in their usual place of residence. What people want is to have quick and easy access to responsive services and trusted care providers when they need them. These principals are universal to both primary and palliative care.
Some of our improvement work will focus on developing palliative care in the community, with providers that people know well. This will extend identification beyond those with cancer. Anyone living with long term conditions and growing frailty would benefit from early palliative care.
But identification is only part of the story.
As important is the coordination of responsive, person-centered services. Services that are delivered through closer, enhanced multi-disciplinary team working. Services that are nearer to people. Services that are geared towards improving continuity between people and their care providers.
You’ll hear more about my work in the coming months. I’d be delighted to learn from your community palliative care initiatives, and to hear your suggestions for improving identification and coordination of palliative care.
Please do get in touch.
Palliative Care: From Diagnosis To Death
The Primary Palliative Care Research Group at the University of Edinburgh have produced a series of videos for people living with declining health and the friends, family members and professionals caring for them.
Early Palliative Care: a video for health and care professionals
This short video aims to help health and care professionals to identify people who are living with progressive illnesses better, to assess their needs in a timely manner and to start discussing and planning future care with them.
Early palliative care improves life’s quality, and in some cases may even prolong life. It promotes realistic medicine, an approach which puts the person receiving health and care at the centre of decision-making.
Clinicians, patients and families can all benefit from carefully integrating early palliative care with on-going treatment, so people can both live and die well.
The information in this video is based on detailed research with patients, families, doctors, nurses and other health and care professionals about people’s experiences living with declining health and dying. ‘Palliative Care from Diagnosis to Death‘ was published in February 2017 in the BMJ.
Key points:
- Identify people early and introduce early, integrated palliative care
- Consider patients’ different dimensions of need at present, and discuss what matters most to them
- Discuss what happens in the different illness trajectories so they know when they might need the most help
- Make an individual anticipatory care plan with patients and families; document, communicate and review this regularly with all involved
There are accompanying notes and suggested discussion questions available here for anyone using the video for teaching purposes.
How to Live and Die Well: a video for the public, patients and family carers
This short video is for everyone. It’s for people who are well just now, but may get a serious illness or life-threatening condition in the future. For people who currently live with progressive illness. It’s also for family members and carers of those who are ill or may become ill, and who want to learn what can happen in the future so they can plan ahead.
The full video, as well as guidance notes and useful links is available here.
There is an extended version for facilitated group viewing and discussion available here.
Strictly Come Dying
This video discusses the different illness trajectories as though each were a dance with a particular tempo and complexity. Just as knowing the dance will help someone dance well, understanding typical physical and emotional sequences of various illnesses help people live and die well.
Our research group in Edinburgh has studied the last year of life in people dying of various illnesses. We found that people dying from different diseases experience dying differently, as each disease trajectory involves different experiences, needs, ups and downs.
Further reading: Palliative Care: From Diagnosis to Death
Welcoming 21 Teams on our Collaborative
Thomas Monaghan, our Portfolio Lead, announces the successful teams on our Living and Dying Well with Frailty Collaborative
We’ve got the key of the door, never been twenty-one before!
21! What a magical number.
It was my age when I met my wife. It’s the name of my favourite Adele album. It’s the name of my favourite card game.
But 21 has a new meaning for me now as we now have 21 teams that are part of the Living and Dying Well with Frailty Collaborative.
21 teams from 19 Health and Social Care Partnerships (HSCP).
21 teams that include over 70 GP practices, but will grow over the next year to include even more practices.
21 teams from across Scotland working together to improve the outcomes for people with frailty who are living in our communities.
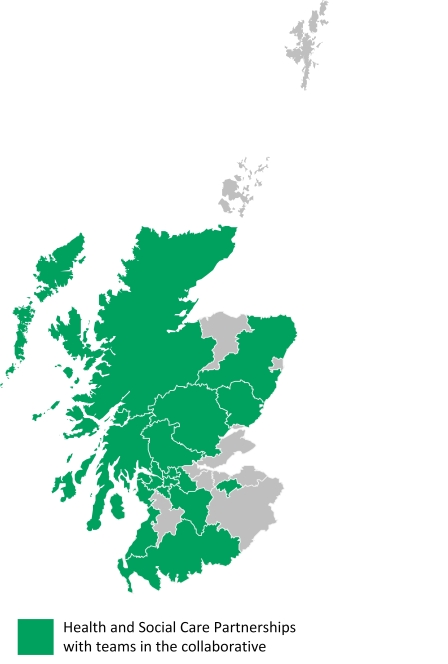 HSCPs with teams in the collaborative:
HSCPs with teams in the collaborative:
Aberdeenshire
Angus
Argyll and Bute
Clackmannanshire and Stirling
Dumfries and Galloway
East Dunbartonshire
East Renfrewshire
Glasgow City
Highland
Inverclyde
Midlothian
North Ayrshire*
North Lanarkshire
Perth and Kinross*
Renfrewshire
South Ayrshire
South Lanarkshire
West Dunbartonshire
Western Isles
*indicates when there are two teams from the HSCP.
Living and Dying Well with Frailty Collaborative
Over the next year we will be working with the 21 teams to improve earlier identification, anticipatory care planning and shared decision-making, to ensure that people living with frailty get the support they need, at the right time, at the right place.
We will do this by helping teams to use tools, evidence and quality improvement methods to:
- find people who are becoming frail before they reach crisis point using the eFrailty Index,
- have anticipatory care planning conversations with people with frailty to understand their wishes for future care, and
- work with a range of health, social care, third sector, independent sector and housing providers in local areas to support people with frailty to achieve what they want for their future.
We welcomed the 21 teams to the collaborative in August and our first Learning Session is in September. The Learning Session will be an opportunity for 21 teams to meet each other and share the work they have already done, learn improvement skills and come together as teams to plan their improvement projects.
The 21 teams have outlined excellent and innovative ideas for their local improvement and we can’t wait to work with them as they implement their ideas over the next year.
21 really is a magical number and together, we’ll change outcomes for people with frailty.
If you want to know more please visit our Living and Dying Well with Frailty webpages or follow us on Twitter. You can get in touch by emailing us at hcis.livingwell@nhs.net, calling us on 0131 314 1232 or tweeting us @LWiC_QI.
Living and Dying Well in Care Homes – meeting with the Care Inspectorate
On Monday 12 August 2019, we were joined at our offices in Edinburgh by members of the Care Inspectorate’s internal palliative and end of life care group. The purpose of the session was to explore how the Living Well in Communities (LWiC) Team could work with the Care Inspectorate to improve palliative and end of life care for people living in a care home.
Why focus on a Living and Dying Well in Care Homes Collaborative?
There are 36000 people living in care homes across Scotland. In 2017 there were 11300 deaths of Care Home Residents. Ensuring that we get this care right for these people is important. (Data from the Scottish Care Home Census, available on the Information Services Division (ISD) website).
Between March 2017 and March 2019 LWiC delivered a programme of work in support of commitment 1 of the Scottish Government’s Strategic Framework for Action on Palliative and End of Life Care. This work highlighted how we could improve palliative and end of life care for residents, their families and people working in care homes.
For example, there was work taken forward by Riverside Care Home in Glasgow which saw the home using the SPAR tool to identify residents with palliative or end of life needs. This led to an increase in the residents with a jointly agreed care plan in place. These care plans help ensure that the wishes and needs of residents are met. From work elsewhere in Scotland we know there is a link between care plans that are shared using the Key Information Summary and being more likely to die outside of hospital. This is explored further in this article. We know that many people want to receive their care at home and this suggests that care planning is helping people have a better experience at end of life.
We would like to spread the learning from this work across Scotland so that other areas are able to benefit from the learning from this work. We think that an improvement collaborative would be an effective way of spreading improvement at scale across a range of areas. However to ensure that the collaborative would be successful we need to develop the content of the collaborative and make sure that there is an appetite for this approach.
To do this we need to engage with other national organisations, health and social care partnerships, care home staff, residents and their families and friends to establish how best to progress this work. We have identified that we must work in partnership with the Care Inspectorate. Hence why we held this meeting on the 12 August.
What did we talk about?
We had great conversations with our colleagues from the Care Inspectorate to share what have been doing so far, reflect on what we had heard and to discuss the scope of the collaborative. A particular issue that became apparent is our differing use of language and terminology, and we will certainly need to build a common understanding of this.
Everyone was really engaged in the session and we came away with some incredibly useful pointers and feedback. Most importantly we started to build some good relationships that will help us move forward with this work in collaboration.
Going forward
We are looking at how we can continue to work together so that we can harness everyone’s expertise. We also need to think about how we can work with care home providers, residents, their families and staff working in care homes.
Undoubtedly we have a lot more work ahead of us over the next year to engage, scope and develop our approach together with the Care Inspectorate.
Our next step is to hold a workshop with a small group of mostly national stakeholders to help us plan the next steps for this work. We aim to continue our conversations to explore how a collaborative, focused on palliative and end of life care in care homes, could make a positive difference to residents, their families and the staff who are delivering their care and support.
If you are interested in discussing this work, have any examples you would like to share, or would like to be kept updated, then please contact: hcis.livingwell@nhs.net.
Please visit our website for further information https://ihub.scot/living-and-dying-well-in-care-homes/
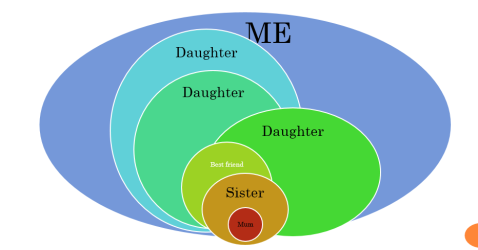
Frailty, palliative care and me
by Tim Warren, Policy Lead for Palliative and End of Life Care, Scottish Government
 My mum lives eight hours away, within earshot of Glastonbury (if only her hearing was a little better). Her frailty is a pressing reality. All of the issues which press in at work – frail older people, most with a host of health issues, increasingly lacking capacity, exhausted family carers, stretched paid carers, the role of GPs, district nurses; it all feels very personal.
My mum lives eight hours away, within earshot of Glastonbury (if only her hearing was a little better). Her frailty is a pressing reality. All of the issues which press in at work – frail older people, most with a host of health issues, increasingly lacking capacity, exhausted family carers, stretched paid carers, the role of GPs, district nurses; it all feels very personal.
As the policy lead for palliative and end of life care at the Scottish Government, I frequently have to answer questions about what I do. I usually begin with how ignorant I was when I took on this role, when I mistakenly thought palliative care was basically about hospices and cancer. Of course, I now appreciate that the lion’s share of palliative care is about supporting frail older people like my mum.
When does care become palliative?
So, good care, provided to people at any stage of their care pathway, becomes palliative with hindsight when the person dies. Specialist palliative care, provided in any setting is clearly ‘palliative’. From this perspective, good care, provided in care homes, or by informal carers, supported by district nurses and GPs, and encompassing the spiritual, social and psycho-emotional and the physical, is also ‘palliative care’.
The strategic framework for action on palliative and end of life care (SFA) starts with support for identifying people who stand to benefit from a holistic palliative approach, highlights the importance of conversations with those people (and those who care about and for them), and then aims to provide coordinated care across all settings.
So, who might benefit from a palliative approach?
At what point does support for people with long term conditions become early palliative care? I have come to think about this in two ways. Firstly, thanks to Kirsty Boyd, consultant in palliative care at Royal Infirmary of Edinburgh, I possess the mental metaphor of “umbrella conversations” – conversations to be carried on, not just when it’s raining, but when it might rain. Such conversations might be initiated with a question like, “If you were to get more unwell, what would it be important for us to know about”. Not having these sorts of conversations early, and recording them in a sharable way, can rob people of care and dignity at the end of life. And, although the National Digital Service will in due course enable such information sharing, at the moment the only available mechanism for reliable sharing across settings is the Key Information Summary.
Secondly, another way of looking at who might benefit is by employing “20:20 hindsight”, and reviewing the profiles and care pathways of those who have died over the most recent available year. In 2017 almost 58,000 people died. Around 16,000 of those died suddenly. Of the remainder around 20,000 died with dementia. This gives an additional significance to having those conversations early.
Why early conversations matter
As a policy team we get to see the letters people send to ministers about the care their loved ones receive. One haunts me. It recounts the last months of the writer’s father’s life, in which he experienced increasing frailty, repeated hospital admissions and disjointed care (along with some examples of kind, warm and compassionate staff). He underwent several operations, repeated burst stoma-bags, unmanaged pain and broken promises of ‘fast-tracked care’. The family said it had seemed like a dreadful rollercoaster, which could have been prevented had they just had a realistic conversation about his likely trajectory, and what mattered to him.
Although not all care pathways are like those of this man, all of those who died expectedly should have benefited from conversations about what mattered to them. Paul Baughan, a GP and the Healthcare Improvement Scotland clinical lead for palliative care, led the development of a new palliative care Directed Enhanced Service, to provide some financial support for identifying those who may be moving towards death. (We worked together on the diagram below). It aims to increase the proportion of those with a KIS at the end of life, but especially people with frailty, who have more often been overlooked.
And it is brilliant to see a focus on ensuring that people in care homes get to benefit from this approach; the work in Edinburgh and Glasgow comes to mind. There is lots still to do, but the support of colleagues in primary care in doing this, and supporting them to do so feels like a key element in making sure that everyone gets the palliative care they need by 2021.
Introducing our Living and Dying Well with Frailty Collaborative

Thomas Monaghan, our Portfolio Lead, discusses our Living and Dying Well with Frailty Collaborative
People in Scotland are living longer than ever before, which is to be celebrated. This means that we all get to spend more time with our loved ones. However, people are not just living longer: they are living longer with more complex health needs and conditions, such as frailty. While we welcome spending more time with our loved ones, we also recognise that it can increase pressure on families, on carers and on our health and social care services to support people to have the best possible quality of life.
Improving care for people with frailty
Supporting people with frailty to have the best possible quality of life is becoming increasingly difficult, as there are growing numbers of older people in Scotland who need support: there will be 25% more people age 65 or over by 2029, and almost 80% more people age 75 or over by 2041.
If we want every older person in Scotland to have the best possible quality of life, then we need to start changing how we support people with frailty to live well in their community.
Our support
At Healthcare Improvement Scotland we want to help health and social care services to make changes so more people with frailty can have a better quality of life in their community. This will help to avoid crises that can lead to poor outcomes and increase pressure on families, carers and health and social care services.
We can do this by helping health and social care services to use evidence and quality improvement methods to:
- find people who are becoming frail before they reach crisis point
- have anticipatory care planning conversations with people with frailty to understand their wishes for future care, and
- work with a range of health, social care, third sector, independent sector and housing providers in local areas to support people with frailty to achieve what they want for their future.
Our Living and Dying Well with Frailty Collaborative
If you want to work with us to help people with frailty to have a better quality of life and reduce pressures on individuals and services, then get in touch. We can talk about how you could be part of our Living and Dying Well in Communities improvement collaborative.
To find out more, get in touch by emailing us at hcis.livingwell@nhs.net, calling us on 0131 314 1232 or tweeting us @LWiC_QI.
Looking forward to hearing from you!
















