 We have recently published a resource that reviews the evidence on continuity and care coordination in palliative and end of life care. This blog post gives an overview of the document and its features.
We have recently published a resource that reviews the evidence on continuity and care coordination in palliative and end of life care. This blog post gives an overview of the document and its features.
Why focus on care coordination?
Good care co-ordination can help to improve people’s quality of life, right up to the end of life.
The Living Well in Communities team has been working with test sites in Dundee, East Ayrshire, Fife, Glasgow City, and Renfrewshire Health and Social Care Partnerships to deliver Commitment 1 from the Scottish Government’s Strategic Framework for Action on Palliative and End of Life Care:
“We will support Healthcare Improvement Scotland in providing Health and Social Care Partnerships with expertise in testing and implementing improvements to identify those who can benefit from palliative and end of life care and in the co-ordination of their care.”
This work is coming to a close in March 2019.
Exploring the evidence on different approaches
Drawing on the priority practices outlined in the World Health Organization practice brief on continuity and co-ordination of care, we identified six key approaches to continuity and care co-ordination in palliative and end of life care:
- Early integrated palliative care
- Collaborative planning of care and shared decision making
- Case management for people with palliative and end of life care needs
- Intermediate palliative care at home
- Technology to support continuity and care coordination
- Building workforce capacity
Working with the Evidence and Evaluation for Improvement Team, we summarised the available systematic-review level evidence on these approaches.
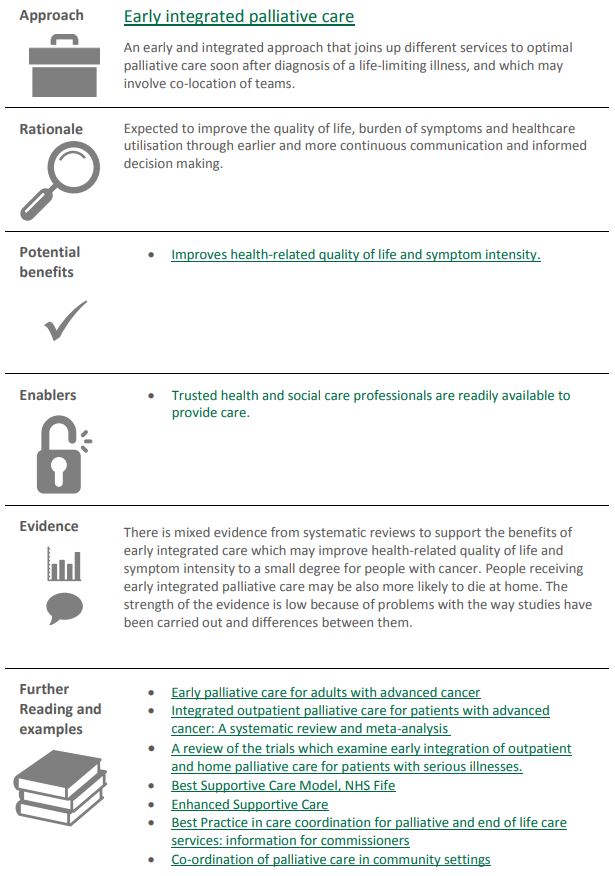
Presenting the evidence visually
As with our Living Well in Communities with Frailty evidence review, we produced visual summaries for each of the approaches. These provide key information on the different approaches to care coordination, and an introduction to the more detailed evidence summaries. The visual summaries include
- a brief description of each approach,
- the rationale behind them,
- the potential benefits,
- enablers,
- brief commentary on the quality of the evidence, and
- links to further reading and examples of local good practice.
We hope that this document will provide a useful overview of the systematic review-level evidence on key approaches to care co-ordination in palliative and end of life care, and highlight the potential benefits of these approaches.
You can access the review, Continuity and Co-ordination in Palliative and End of Life Care: evidence for what works by clicking on the document image below: